Abstract
Background:
Burkitt lymphoma/leukemia (BL) is a highly aggressive mature B-cell neoplasm with multiple subtypes differing in their demographic and geographic presentations. Prompt diagnosis and referral of BL patients is key towards its prognostic advantage and hence its outcomes could be vulnerable to social and healthcare inequities.
National data on the epidemiology of cancer are commonly reported by broad racial/ethnic categories, such as "Hispanic." However, few studies have disaggregated Hispanic (HI) groups and explored mortality differentials in this heterogeneous population. (J Immigr Minor Health. PMID: 18506623)
The HI population in Florida (FL) is primarily of Cuban ancestry, as opposed to the primarily Mexican background of Texas (TX) (Front Public Health. PMID: 30234082). Both the FL and TX populations have similar stress factors, such as immigration and education/job opportunities that may affect patients, but because the two areas are demographically and culturally unique and have different genetic admixtures, it's possible their outcomes in certain cancers could be different. The present study aimed to use data from two large population datasets that comprise majority of HI with different ancestry, to provide an update on the incidence and mortality differentials in patients with BL when compared to Non-Hispanics (NH) over the past decade, between 2006 and 2017.
Method:
This is a retrospective study of patients >18 years diagnosed with BL from the Texas Cancer Registry (TCR) and the Florida Cancer Data System (FCDS) from 2006-2017. Patients were identified by the International Classification of Diseases for Oncology Third Edition (ICD-O-3) code list. All patient data was obtained de-identified and standard demographics, variables and treatment effect were analyzed. The significance of variation in the distribution of categorical outcomes within ethnicity (HI, NH) was assessed with Fisher's Exact tests or Pearson's Chi-square tests as appropriate; age was assessed with T-tests or Wilcoxon tests as appropriate. Survival distributions were described with Kaplan-Meier curves and significance of variation in median survival with ethnicity was assessed with log rank testing. All statistical testing was two-sided with a significance level of 5%.
Results:
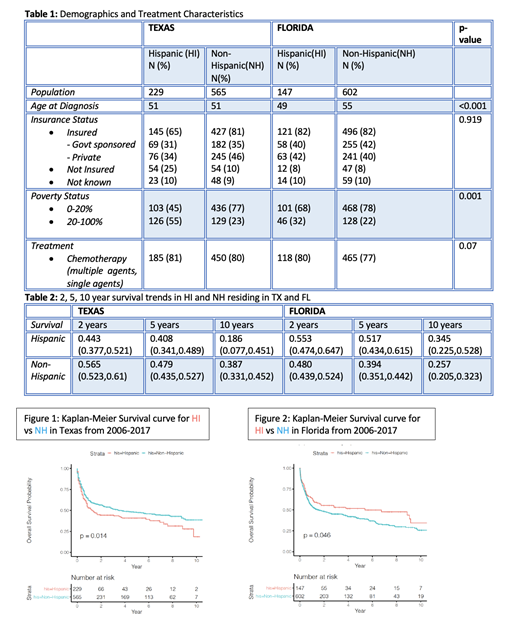
A total of 1543 patients (794 from TX and 749 from FL) were included in our analysis. HI comprised of 29% (n=229) of TX registry and 20% (n=147) of FL database. Consistent with known age and gender epidemiology of BL, younger males were commonly affected in both ethnic groups regardless of the geographic region, except for slightly younger age at diagnosis in HI in FL (49 years(y)) when compared to NH (55 y, p = <0.001).
While TCR reports ancestry, FCDS does not report it. Majority of HI in TX are of Mexican origin (20%) with larger population grouped under "Spanish, NOS/Hispanic group"(73%). HI in TX and FL suffered from higher percentage of poverty when compared to NH (20-100%: 55% vs 23% in TX and 32% vs 22% in FL respectively). In terms of health insurance coverage, HI in TX were under-insured when compared to NH (65% vs 81%) but HI and NH had equal health coverage in FL. (82% vs 82%) (Table 1)
The median survival time was longer for HI in FL (5.4 y vs 1.6 y) but shorter in Texas (1.2 y vs 3.4 y) when compared to NH. The 2, 5, 10 year survival trends in HI and NH residing in TX and FL are shown in Table 2. The 10 y Overall Survival (OS) of HI from FL was statistically better when compared to NH (p=0.046) whereas HI had inferior survival to NH in TX (p=0.014) (Figure 1 & 2).
Conclusion:
Outcomes of BL in HI population in FL appears unique when compared to TX. HI in FL were younger with longer median survival and superior OS when compared to NH. However, HI in TX had an inferior OS when compared to NH. Whether these disparities are a reflection of higher rates of poverty and lack of insurance among H in TX compared to H in FL or if related to national origin and/or age and environmental factors remains to be determined. This study illustrates that outcomes of cancer could vary by HI subgroups. Examining HI by nativity and country of origin may help identify risks specific to individual subpopulations and is needed if health disparities are to be adequately identified, understood and addressed.
Diaz Duque: Incyte: Consultancy; Morphosys: Speakers Bureau; Astra Zeneca: Research Funding; Hutchinson Pharmaceuticals: Research Funding; Epizyme: Consultancy; ADCT: Consultancy.